游敬孝 陳博光教授
青少年特發性脊椎側彎的治療有長足的進展。尤其利用椎弓釘之插入椎體內的方式來矯正效果相當好、也就是說矯正校率遠比過去的矯正器材更令人滿意。我們僅將過去所做的成績、既術後五年底以上之中期隨訪結果之文章(登載於Scoliosis雜誌2012年)、供有意者參考。
內容部分摘要:
一、研究方式
從2001年到2003年, 總共有49位特發性脊椎側彎的病人接受全椎弓釘矯正手術,包括38位女性及11位男性, 他(她)們手術時平均年齡為18.5±5.0歲, 平均隨訪的時間為6年(5.1–7.3 年)。根據King式分類, 第一型10位,第二型 16位,第三型20位, 其餘第四型1位及第五型2位。每一位病人評估方式包括:術前, 術後及最後隨訪之柯氏角(Cobb angle),彎度矯正率(correction rate),矯正喪失率(correction loss rate),併發症,矢狀面(sagittal plane)及椎弓釘準確率(pedicle screw accuracy rate)。此外,我們還使用台灣版SF-36問卷來評估術後病人的整體身心及社會功能狀態。
二、結果
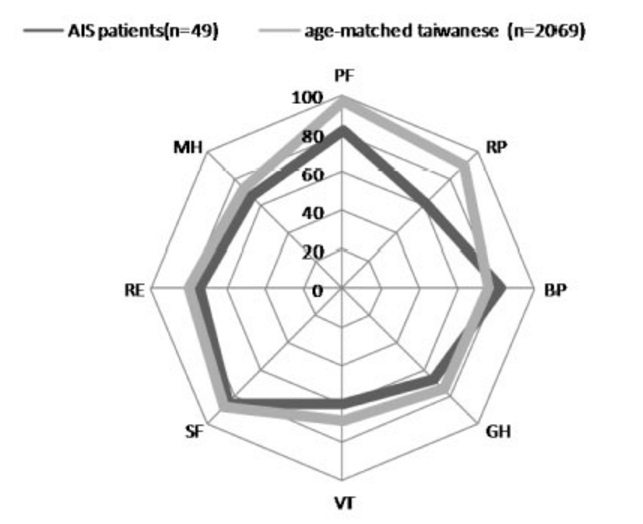
術後柯氏角從平均58.0±13.0度進步到16.0±9.0度,而最後隨訪時為18.4±8.6度。這代表?72.7%彎度矯正率及3.92%的矯正失率。胸椎駝彎(thoracic kyphosis) 從22±12度降到20±6度; 而腰椎後凸(lumbar lordosis)維持在正常範圍內 (37.0±12.0度)。另外,除了一位病人在術後併有血胸的發生,其餘並無重大的併發症產生。此系列共植入831根椎弓釘,約有56根(6.7%)的位置稍微外偏,但都未造成神經或血管的傷害,也沒再次改變椎弓釘的位置。與同年齡台灣其他2069位民眾比較SF-36分數,這些脊椎側彎的病人在生理功能(physical functions)及 生理角色(physical role)這兩面向,有著較低的分數。
三、結論
以全椎弓釘手術方式治療青少年特發性脊椎側彎,是有效且安全的方法。其成效良好、而且有72%以上之矯正率。對其他更嚴重的病友、也同樣有效。目前已經有近千例的經驗。
Segmental correction of adolescent idiopathic scoliosis by all-screw fixation method in adolescents and young adults. Minimum 5years follow-up with SF-36 questionnaire
Ching-Hsiao Yu,Aff1 Aff1 Department of Orthopaedic Surgery, Tao-Yuan General Hospital, No.1492, Zhongshan Rd, Taoyuan City 330, Taiwan, (R.O.C.)
Keywords Adolescent idiopathic scoliosis (AIS), All-screw method, SF-36 questionnaire. BackgroundIn the past decade, pedicle screws have become the mainstream of the fixation method used to correct spinal deformities. Surgical treatment of adolescent idiopathic scoliosis (AIS) with an all-screw method has also proven to be a effective and safe procedure [1-3]. Compared with other spinal fixation devises, pedicle screws have greater correction power because of their three-column fixation [4,5]. In our experience, the use of the all-screw method achieves a superior three-dimensional curve correction rate than the two previous methods: the all-hook method and hook/screw hybrid method [6,7]. Additionally, more motion segments could be saved by reduction of the fusion length in thoracic scoliosis [1]. However, the insertion of pedicle screws in the thoracic spine is always a safety concern, especially in the upper thoracic area because of small pedicle calibers, close anatomical relations to adjacent neural structures, and deformed anatomical structures [8,9]. While it has been claimed that the insertion of pedicle screws, even with free-hand technique, is rather safe [2,8], complications such as nerve root injury and durotomy associated with screw placement have been reported [9,10]. As a result, the treatment of idiopathic scoliosis with In our institution, the fixation technique in treating idiopathic scoliosis was shifted from hybrid fixation to the all-screw method beginning in 2000. We have observed an improved correction rate and minimal complications. We presume that all-screw construct could provide a good three-dimensional curve correction and maintenance. The purposes of the current study were to evaluate the intermediate-term (>5 years) effectiveness and safety profile of the all-screw fixation method in the treatment of idiopathic scoliosis. The functional outcome and quality of life was assessed by means of an established questionnaire. MethodsPatientsThe study was approved by the local ethics committee. Forty-nine AIS patients (38 females, 11 males) were retrospectively evaluated during a consecutive series from September 2001 to December 2003. Patients with congenital scoliosis, neuromuscular scoliosis and those who had undergone revision surgeries were excluded. The minimum follow-up was 5 years (mean, 6.1 years; range, 5.1–7.3 years). All patients were operated on by the senior surgeon (PQC) and the first author (CHY) in a single institution with the all-screw method. The mean patient Table 1 Patient Demographics and Operative Data
* Data are expressed as mean, with range in parentheses; there were no significant differences between the two groups except in age of operation and Risser grade; ADIS adulttype adolescent idiopathic scoliosis Patients were further divided in two groups, depending on the age of surgery: the adolescent (AIS) group ( ≤20 years, n=34) and the young adult (ADIS) group (> 20 years, n=15). The patient demographics in the AIS and ADIS groups were similar except the age of surgery and Risser grade (Table 1). The mean age at surgery for the ADIS patients was 25.0±3.2 years (range, 20.0 to 31.4 years) while those in the AIS patients was 15.6±1.9 years (range, 11.7 to 19.8 years)(p<0.05). The mean Risser grade for the ADIS group was 5.0 whereas for AIS group was 3.2±1.4 (p<0.05). The curve classifications was similar between two groups with thoracic curves were predominant. ProceduresPedicle screws are inserted on the concave side one by one from the lumbar up to the thoracic segments. Then the screws are inserted to the convex side, ranging in every other segment from lower to the uppermost segment. We prefer inserting 2 screws each in the lower and uppermost adjacent 2 segments. At this stage, plain X-ray films are taken both in the AP and lateral views to confirm the exact positions of the screws in most of the patients. But in some patients, these films are taken after completion of the corrective procedures. The contoured rods are linked to the rods by vertical tapping on the rods into the heads of the screws on each side. Facetectomies are also performed in each segment. Derotation is started on the concave side first after completion of connecting rod to the screws. This procedure is finished after rotating the rod to the vertical position as seen from the top. Only mild distraction of the screws is necessary. Actually, due to segmental insertion of the screws, distraction procedure is not possible. In the lower lumbar scoliotic ends, due to its convexity, compression between screws can be performed. Then the same procedure is performed on the convex side. One or 2 cross links are placed, one in the upper and the other in the lower part of the construct. With proper decortication of the laminae, the bone chips are placed on them. In our cases, we use cancellous allogenous bone graft taken from bone bank for fusion. Thoracoplasty is considered and carried out only when the rib protrusion is obvious and the angle of trunk rotation (ATR) is greater than 15°. Among the 49 cases, 42 underwent a one-stage posterior spinal fusion (PSF) and seven underwent a two-stage operation; the latter consisted of an anterior spinal fusion followed by posterior spinal fusion (APSF) with instrumentation. Four patients had additional thoracoplasty. The average number of fused spinal segments was 10.8 (range, 8–13). In this series, the screw system used included the Universal Posterior System (UPS; Aaxter, Taipei, Taiwan) for 45 cases, the Moss-Miami (DePuy Spine, Raynham, MA, USA) for 2 cases, and the Diapason (Stryker, Kalamazoo, MI, USA) system for the remaining 2 cases. The titanium-made UPS system has 6.5, 5.5 and 4.5 mm diameter screws of different lengths. The rod was 6.0 mm diameter with a smooth surface. As much as possible, mono-axial screws were used because the correction power can reach from posterior bony part to the anterior body portion [14]. Apical trunk rotation (ATR) was presently assessed using the forward bending test at preoperative (PreOP) and final follow-up (FFU) period. The three parts of the ATR were recorded including thoracic level (TH), thoracolumbar level (TL) and lumbar level (L). Spine radiographic assessment included standing postero-anterior and lateral radiographs at PreOP), 1 week postoperative (PO) and at FFU. The passive standing lateral bending films were taken before surgery to measure curve flexibility. Three-dimensional deformity of each patient was assessed. Major and minor curves on the coronal plane were measured by the Cobb method. The sagittal alignment included the thoracic kyphosis from T4 to T12, and lumbar lordosis from L1 to L5. Rotation of the apical vertebra was determined by the Nash and Moe method on standing postero-anterior films [15]. The rotational correction of the apex of the curve was assessed by comparing the PreOP and PO rotational deformity of the apical vertebra. In cases where the pedicle of the apical vertebra was obscured by the inserted pedicle screw, the rotations of adjacent uninstrumented vertebral (superiorly or inferiorly) were compared. There are no cases in which the apical vertebrae and adjacent ones instrumented with pedicle screws which obscure the pedicle. The curve correction rate of all three planes, loss of correction rate and numbers of fused segments were analyzed to evaluate the effectiveness and maintenance of operation. Complications and malposition rates of the pedicle screws were documented to ascertain the safety profile. The positions of pedicle screws at every instrumented vertebral level in the 1-week PO postero-anterior and lateral radiographs were studied. This was performed by an independent spinal surgeon who was not involved with this study. The outcome of the evaluations was assigned as intrapedicular or extrapedicular placement. Extrapedicular placement was further categorized into inferior, superior, lateral or medial position. Functional outcome was assessed using the SF-36 questionnaire (Taiwan version 1.0) [16] at the latest follow-up. Because of the lack of preoperative data, we also compared this data to an age-matched population of 2069 individuals in Taiwan [16]. We also separate the results by AIS and ADIS patients. The age at follow-up is averaged 24.2±4.5 years (range, 17.2–36.6 years) while 2 patients were aged under 18 years at follow-up Statistical analysisThe T-test was used with level of significance of 5% (p<0.05) to compare the differences between PreOP, PO and FFU data. ResultsCoronal plane correctionIn the coronal plane, the PreOP Cobb angle of the major curve was 58.0±13.0° (range, 40– 107), which was corrected by 72.7% to 16.0±9.0° (range, 5–51) (P<0.0001)after surgery (Table 1). The PreOP Cobb angle of the compensatory curve was 38±10° (range, 20–64), which was corrected by 72.4% to 11±8° (range, 0–26) (P<0.001) after surgery. The mean correction loss for major curve of all 49 patients at FFU was 2.4o (3.92%) (Table 2). Table 2 Coronal and Sagittal Parameters Results
data are expressed as mean±standard deviation;*significantly different from preoperative data; ** significantly different from postoperative data Preop preoperative, PO postoperative, FFU final follow-up, CR correction rate, CLS correction loss rate Sagittal curve correctionThe mean preoperative thoracic kyphosis (T4-T12) of 22±12° (range, 0–50) was reduced to 18±7° (range, 3–37) (P<0.001) after surgery and to 20±6° (range, 5–35) (P=0.12) at FFU. The mean preoperative lumbar lordosis (L1-L5) was decreased from 37±12° (range, 60–5) to 33±10°(range, 63–12) (P<0.001) after surgery, and to 37±12° (range, 63–12) (P<0.005) at FFU (Table 2). Ten out of the 49 patients had thoracic hypokyphosis preoperatively (≤10o). They achieved better kyphotic alignment after the index procedure (mean, from 6.5±3.5° to 12.8°±5.3). (P<0.005). The mean angle improved to 18.6±6.9° degrees at FFU (P<0.005). Of these 49 patients, four had thoracic hyperkyphosis (≥40). The mean preoperative thoracic kyphosis angle of 45.8±3.0° (range, 43–50) was reduced to 24.0±9.0° (range, 15–36) (P<0.001)after the operation and to 22.0±1.8° (range, 20–24) (P<0.005) at FFU. Axial plane correctionThe mean preoperative ATR was reduced from 7.8±5.0° to 5.6±3.8° (TH level, P=0.28), from 8.8±5.0° to 6.3±4.1° (TL level, P=0.15), and from 8.9±5.2° to 3.1±3.5° (L level, P<0.001) at FFU. The mean Nash and Moe grade of PreOP apical vertebra rotation of 2.1±0.8 was improved to 0.7±0.8(P<0.01), but increased to 0.8±0.8 at FFU(p=0.45) (Table 3). Table 3 Axial l Plane Parameters Results
data are expressed as mean±standard deviation;*significantly different from preoperative data Insertion accuracy of pedicle screwsA total of 831 pedicle screws were inserted, which included 596 thoracic and 235 lumbar screws. The mean number of pedicle screws inserted per patient was 17 (range, 10–24). Among the 831 pedicle screws, 56 (6.7%) were found to be malpositioned and most of them were situated in the thoracic spine (42/56, 75%). Furthermore, 16 screws were found inferiorly, 25 found laterally, and 15 superiorly to the pedicle. None of them were found medially. Fortunately, there were no patients who sustained a nerve root injury during surgery. ComplicationsThere were no neurological deficits, visceral or vascular injuries after the operation and during the admission course. Also, there were no instrumentation failures or pedicle screws pull-out at the latest follow-up. One patient developed an anesthesia complication of right hemopneumothorax after central venous line insertion. The hemopneumothorax resolved uneventfully after chest tube insertion. Short-form 36 (SF-36) questionnaire findingsAll 49 patients completed the SF-36 questionnaire. We calculated their scores by using the scoring algorithms and data entry criteria provided by the SF-36 Health Survey Manual. The scores were then averaged to develop norms in each category: Physical Functioning scale (PF)=81.94, Role Physical scale (RP)=61.29, Bodily Pain scale (BP)=82.42, General Health (GH)=67.26, Vitality scale (VT)=60.48, Social Functioning scale (SF)=85.08, Role Emotional scale (RE)=75.01, and Mental Health scale (MH)=67.59. The Physical Component Summary (PCS) was 48.49±6.52 while the Mental Component Summary (MCS) was 48.32±7.03 (Table 4). Compared with the 2069 age-matched Taiwanese, we found significantly lower SF-36 scores of these AIS patients in two variables: physical function (81.94 versus 96.82), and role physical (61.29 versus 89.63) (Figure 1). We further compared the SF-36 scores between AIS and ADIS groups (Table 5). Among them, AIS group had nonsignificant lower scores in two variables: role physical scale (53.75 versus 75.00, P=0.76) and role emotional scale (69.99 versus 84.13, P=0.63). The Physical Component Summary (PCS) and Mental Component Summary (MCS) between these two groups were similar. (PCS: 48.29 versus 49.96, P=0.26, MCS: 48.80 versus 47.45, P=0.65) Table 4 SF-36 Scores of 49 AIS Patients
Data are expressed as mean, with range in parentheses Figure 1 Comparison of SF-36 scores between 49 AIS patients (black line) and 2069 agematched Taiwanese (grey line) showed lower scores in PF and RP variables of AIS patients. PF=Physical Function; RP=Role Physical; BP=Bodily Pain; GH=General Health; VT=Vitality scale; SF=Social Function; RE=Role Emotional; MH=Mental Health Table 5 Comparision of SF-36 Scores Between AIS and ADIS Pateints
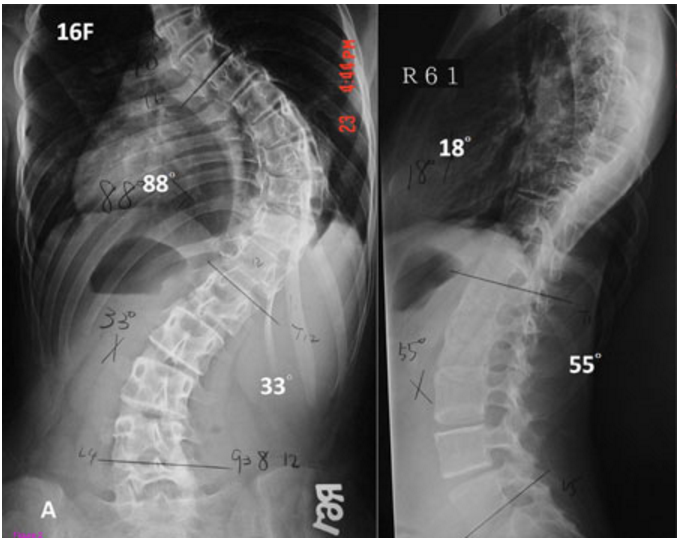
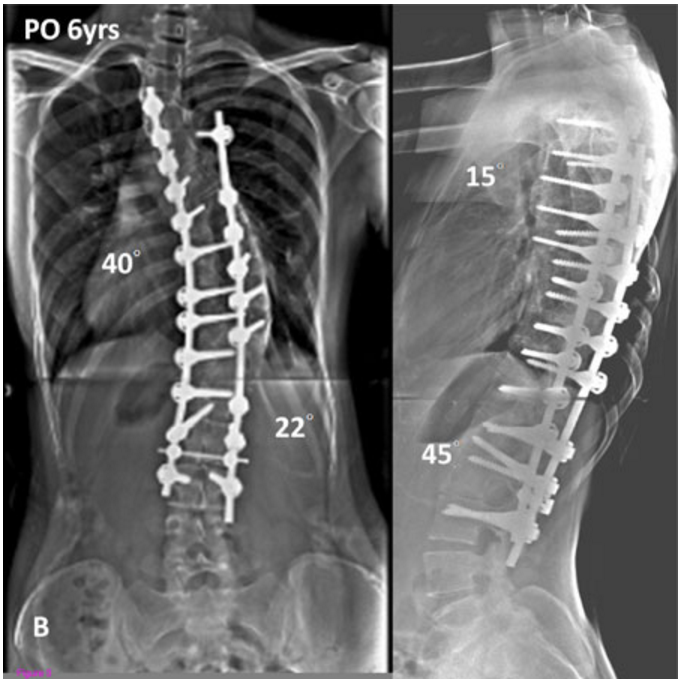
AIS adolescent idiopathic scoliosis; ADIS adult-type adolescent idiopathic scoliosis DiscussionAlthough some controversy does exist, the all- screw construct has gained worldwide popularity in treating idiopathic scoliosis in the last decade. This reflects the majority consensus that the all pedicle screw approach can achieve better three-dimensional correction and less correction loss compared to the all-hook and hybrid construct approaches. A direct comparison between the hybrid and all-screw construct revealed superior major curve correction in all-screw group (70% versus 56%) in 58 AIS patients [7]. This is consistent with a previous study using the Moss-Miami hybrid construct in 61 AIS patients, which revealed a 56% correction rate of the major thoracic curve [17]. In the present study, a correction rate of 72.7% was achieved on the coronal plane with a flexibility of 41.8% (Figure 2). This correction rate echoes those of other studies on segmental pedicle screw fixation of idiopathic scoliosis [1,3,7]. Figure 2 A, Preoperative AP, and lateral radiographs of a 13 year-old-female with 1A curve. B, The patient underwent anterior fusion followed by posterior spinal fusion from T3 to L3 with all-screw construct. Postoperative radiographs of 6 years followup showed 55% correction rate Correction loss of the major curve with various types of instrumentation has been given great attention in the literature. Improvements in the fixation instruments used in scoliosis surgery have improved the correction loss rate. In one study, for example, the use of CD instruments in 64 patients produced an average correction loss for King type 2 and 3 curves of 5.2o (11.6%) and 3.9o (8.3%), respectively [18]. The use of pedicle screws, which can provide better holding power, can substantially improve the correction loss rate from 3–6% [3,7]. In this series with minimum 5 year follow-up, the correction loss averaged 2.4o (3.9%). Compared to our own previous reports with 7.8% correction loss rate for all-hook and 6.6% for hybrid construct [19], we presently obtained a better result. Also, this compares favorably with other intermediate-term studies using segmental screw instrumentation [1]. The results of long-term follow-up of Harrington rod instrumentation for correction of idiopathic scoliosis highlights the importance of preserving or restoring sagittal alignment of the spine PO. Numerous reports have pointed out the complications of significant loss of lumbar lordosis, which results in “flat-back syndrome” [20]. In this study, the thoracic kyphosis and lumbar lordosis were well-maintained PO and at the latest follow-up. In addition, the thoracic hypokyphosis and hyperkyphosis in our 14 patients improved to a better kyphotic angle. The same effect has been reported in a screw group with good correction of preoperative hypokyphosis (from 9o to 27o) [6], which was comparable to the hook or hybrid groups. In another study, the PreOP hyperkyphotic status in 26 patients was reduced in the screw group [21]. Safety on insertion of thoracic pedicle screws is always a great concern [2], especially at the concave upper thoracic segment with the deformed and small caliber pedicles. Although the incidence is rare, the complications of thoracic screw misplacement can be obvious and fatal. Reported complication rates associated with pedicle screw placement range from 0–25% [10], in which the malposition of the screw is the most common problem. In addition, major complications such as neurologic or vascular injury are exceptionally rare. In our series, the screw misplacement rate was 6.7%. Also, there were no major or fatal complications. Therefore, we consider that placement of thoracic pedicle screws using free hand technique is a safe and reliable technique. But, the technique requires experienced personal with better tactile feedback skills and a thorough understanding of the deformed spine anatomy. The technique additionally benefits from the more user-friendly instrumentation tools developed in recent years. These included a smaller pedicle finder (2 mm) and various choices of pedicle screws for upper thoracic segments (25 mm, 30 mm, and 35 mm long). While we did not use the navigation system for pedicle screw placement, we think this modern modality could be helpful for deformity operations. Short form-36 (SF-36) and Scoliosis Research Society (SRS) Outcomes Instrument (SRS-22) are both well-validated questionnaires of “quality of life” assessment[22,23]. Although a Chinese adaptation of the SRS-22 has been previously validated in Hong Kong, no validation exists for use in Taiwan. SF-36, on the other hand, has been validated and used in Taiwan since 1996 (Taiwan version 1.0) [24]. The SF-36 health status questionnaire is a patient elfperceived tool and has been documented in several studies when assessing functional status of scoliosis patients [22,23]. Physical and mental status is also very crucial for these young patients, who are usually students or young employees with many physical and social activities. In the present study, there were two significantly lower scores compared to agematched Taiwanese including physical function (PF), and role physical (RP). It is notable that both variables belonged to the physical health category. This indicates that, even with similar mental health compared with healthy populations, such patients subjectively demonstrate inferior physical status and role limitation. This is consistent with a Norway study with 30 AIS patients [25]. Limitations of this study include relatively small sample sizes and no omparative groups. We also did not use CT scan to assess the accuracy of screw placement. However, this study demonstrates the early experience and clinical results of using all-screw method by a single surgeon in a single institution. ConclusionsBased upon the results obtained from this review of 49 AIS patients with minimum 5 years of follow-up, we suggest that the all-screw method is efficient and safe. The outcomes in threedimensional correction are satisfactory and comparable. The curve maintenance is good with minimal loss of correction. Compared with age-matched healthy populations, these patients did present some limitations on their physical health, as assessed by the SF- 36 questionnaire. Competing interests One or more of the authors have received funding from NSC Grant Authors’ contributions CHY, SCM and CHP participated in the design of the study and performed the statistical analysis. CHY and PQC conceived of the study, and participated in its design and coordination and helped to draft the manuscript. All authors read and approved the final manuscript References
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
游敬孝 陳博光教授

